There are nine kinds of muscular dystrophy and of these, Duchenne MD is the most common severe form of childhood MD. It affects about 1 in 5000 newborn males, only in very rare cases has it affected females. DMD is a genetic disorder that causes progressive muscle degeneration and weakness. Patients usually die by age 30 to 40.
DMD is caused by the absence of a protein, dystrophin, that helps keep muscle cells intact. In 1986 it was discovered that there was a gene on the X chromosome that, when mutated, lead to DMD. Later, researchers discovered that the protein associated with this gene was dystrophin. From this information, we can tell that this disorder is sex-linked, which explains why women are mainly carriers.
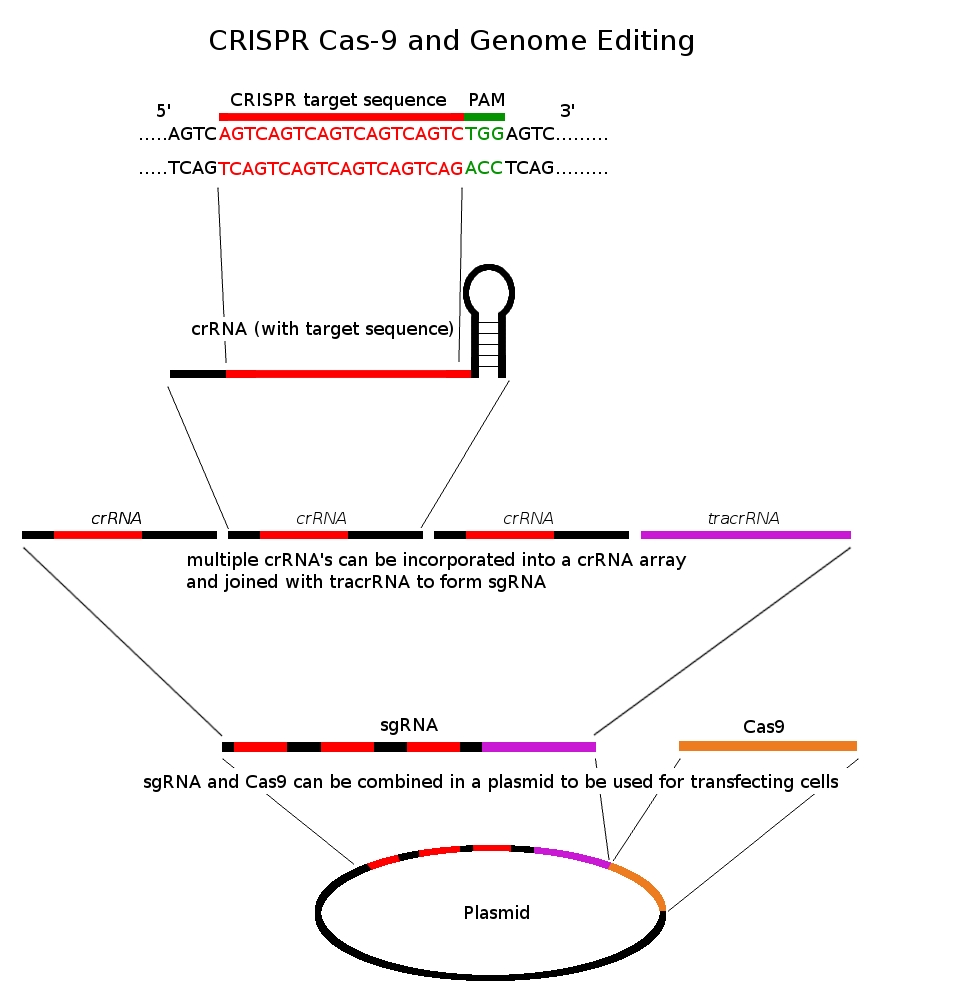
No one has found an absolute cure for this genetic disorder until now. Even in recent years, people have discovered treatments that will make patients’ lives more bearable, but never reverse the disorder. As a result of these advances, mostly in cardiac and respiratory care, patients are able to live past teen year and as long as in to their fifties, though this is rare. Although there are still drugs being tested like Vamorolone (a “dissociative steroid,” is an anti-inflammatory compound), more treatments on the molecular level are now being considered. However, thanks to recent discoveries and research with the new genetic technology, CRISPR/ Cas9, scientists may have found a treatment for DMD.


Leave a Reply