In the United States, there are currently more than 10,374 patients hospitalized per week who tested positive for COVID-19. 15% of these patients are in the ICU (Intensive Care Unit). As of November 4, the test positivity rate is 8.5%. When the test positivity is above 5%, this indicates that transmission is considered uncontrolled.
Due to the fact that many people are using home tests that are not reported through public health or are not testing at all, the official case counts underestimate the actual prevalence of COVID-19.
The dominant variant nationwide currently is HV.1, with 29% of cases, followed by EG.5, with 21.7% of cases and FL.1.5.1, with 9.3% of cases. HV.1 was documented by the Centers for Disease Control and Prevention (CDC) in low numbers during the summer. However, now that the strain has the highest prevalence of any, it claims responsibility for more than a quarter of new coronavirus cases in the U.S. as of late October.
This strain is still a sub-variant of omicron, as is every strain that is in circulation. This strain is a descendant of EG.5, which is the second most common variant in the U.S.
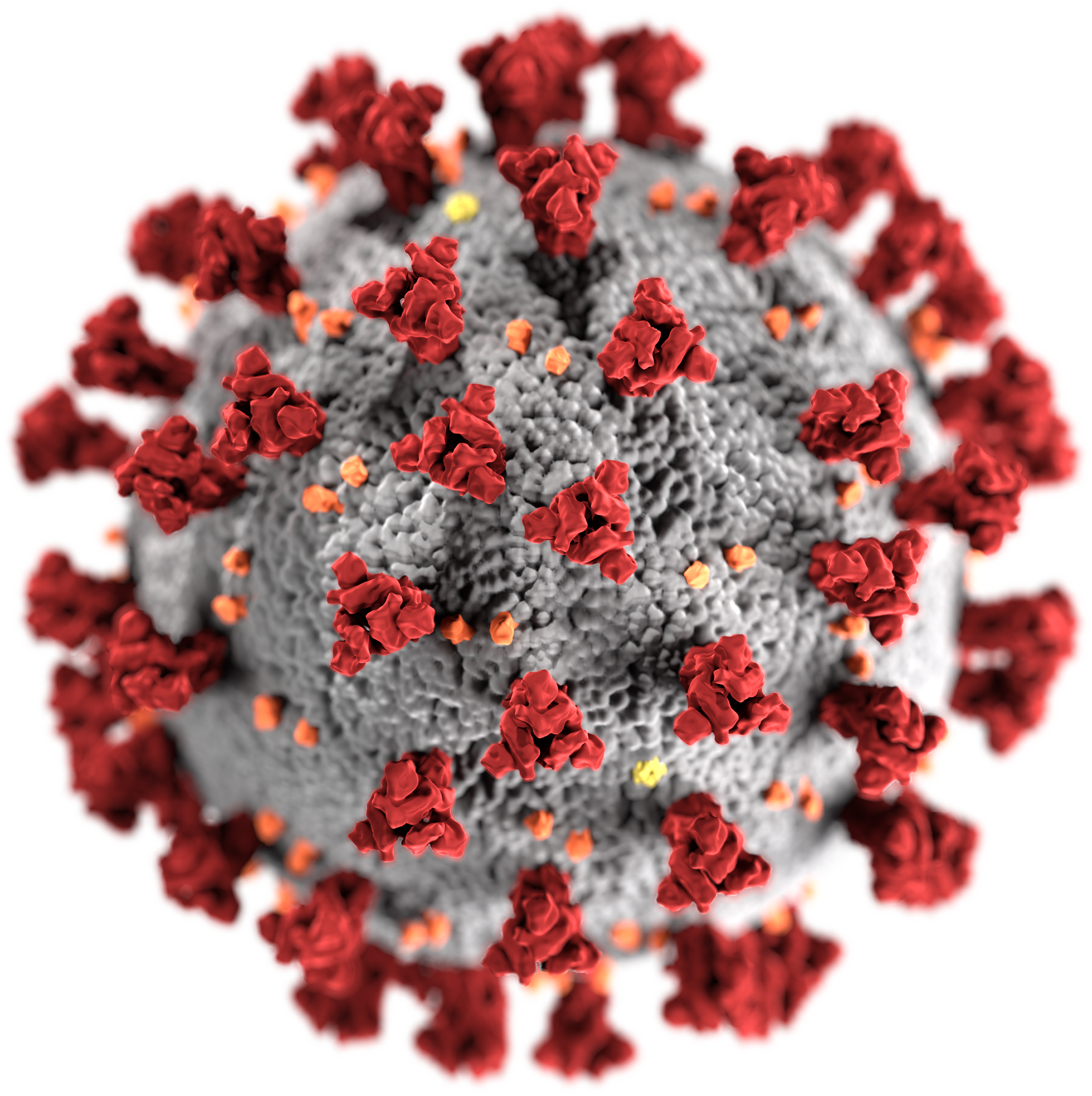
HV.1 is highly infections. The emergence of HV.1 shows how the SARS-CoV-2 virus, which causes COVID-19, is able to mutate and cause new, highly transmissible variants. The symptoms of HV.1 are very similar to those caused by recent variants of omicron.
Omicron S exhibits a heightened dependence on a significantly elevated level of host receptor ACE2 for effective membrane fusion compared to other variants. This characteristic may elucidate its unanticipated cellular tropism. The mutations not only reshape the antigenic configuration of the N-terminal domain of the S protein but also modify the surface of the receptor-binding domain in a manner distinct from other variants. This alteration aligns with its notable resilience against neutralizing antibodies. These findings imply that Omicron S has developed an exceptional capacity to elude host immunity through an abundance of mutations, albeit at the cost of compromising its fusogenic ability.
The Omicron variant of the SARS-CoV-2 virus introduces a distinctive challenge to the immune response system, primarily through mutations in the spike protein. These alterations in the antigenic configuration of the spike protein have raised concerns about the potential impact on the effectiveness of the immune response, particularly with regards to neutralizing antibodies generated from prior infections or vaccinations. The unique genetic makeup of Omicron may allow the virus to partially evade recognition by existing antibodies, potentially leading to breakthrough infections. Moreover, the variant’s influence on cellular immunity, mediated by T cells, is still under investigation, but T cell responses may play a crucial role in controlling infections even if antibody responses are compromised. The evolving nature of the virus underscores the importance of public health measures, including vaccination campaigns and booster shots, to adapt to the changing landscape of the pandemic and reinforce the immune system’s ability to respond to new variants like Omicron. Ongoing research is essential to comprehensively understand the implications of Omicron on the immune response and to inform effective strategies for mitigating its impact on public health.
Omicron stands out with approximately 50 mutations, surpassing the mutation count of any prior SARS-CoV-2 variant. Among these, 32 alterations are within the spike protein, the primary target for most vaccines aiming to neutralize the virus. As of December 2021, numerous mutations in Omicron were novel and distinct from those observed in earlier variants. By April 2022, the variant exhibited 30 amino acid changes, three small deletions, and one small insertion in the spike protein when compared to the original virus. Notably, 15 of these changes were situated in the receptor-binding domain (residues 319–541). As of December 2022, the virus featured additional modifications and deletions in various genomic regions. For instance, three mutations at the furin cleavage site, crucial for its transmission, were identified.
Health officials are not concerned with the latest variant. This is because it appears that HV.1 is very similar to EG.5, also known as “eris.” They are so similar that the World Health Organization (WHO) does not separate the two in its estimates. Globally, Eris is the most prominent strain, accounting for 46% of global cases as of late October, according to the WHO. This estimate also includes cases from HV.1 and another similar strain, HK.5.
HV.1 does not appear to cause more severe illnesses. However, it is expected that it brings the same high transmissibility that eris has. More cases will cause more variants with more mutations to occur.
Dr. Perry N. Halkitis, the dean of Rutgers School of Public Health, says that “the concern about the multitude of mutations is that it is likely and possible that there are versions of the virus that will be more evasive to the immunity that people have.”
However, the fact that HV.1 is so similar to EG.5, the updated coronavirus vaccines are expected to work on the new strain.
However, the shots’ advantages are limited by low uptake so far. Only about 7% of U.S. adults and 2% of children got the new COVID-19 vaccines during the first month it was available, according to national surveys. Despite the rollout being hampered by availability and insurance issues, U.S. health officials say those problems have been mostly resolved.
Surveys also found that almost 38% of adults and parents said that they probably or definitely will not get the shot for themselves or their children.
Hesitancy and vaccine fatigue are surely large parts of the uptake problem. When it comes to COVID-19, there is a general lack of urgency now that vaccines and treatment are widely available.
Halkitis says, “we’ve opened a window of opportunity for people who are resistant to vaccination to begin with to say, ‘Well, it doesn’t look so bad anymore, so I’m just going to bypass it.’ Just like how they react to the flu.”
According to CDC data, COVID-19 weekly hospital admissions have been decreasing or stagnant for nearly two months. However, these numbers remain elevated at more than 15,700 new admissions for the last full week in October, more than double summer’s low of about 6,300 in June.
With the upcoming cold winter months approaching, scientists are anticipating more COVID-19 infections as cold temperatures push people indoors.
Halkitis says that, “I expect there to be more rapid spread as is the case with any respiratory virus in the winter months.”
The CDC is predicting that a moderate COVID-19 wave will sweep over the U.S. according to its respiratory disease season outlook.
The CDC said in an update to its respiratory disease season outlook published last month that, “COVID-19 variants continue to emerge but have not resulted in rapid disease surges. We continue to anticipate a moderate COVID-19 wave, causing around as many hospitalizations at the peak as occurred at last winter’s peak.”
Scientists anticipate that the variants circulating in the U.S. will continue to change as the virus spreads and adapts to its environment.
Halkitis says, “The more we spread it to each other, the more it’s going to keep replicating in people’s bodies, the more likely it will be that mutations are going to occur.”
Based on these findings, I am not very concerned about COVID-19 mutations and variants. Having recently received the COVID-19 booster, I feel great and confident in the effectiveness of the vaccination. In my view, the pandemic no longer appears to be a national emergency. What are your thoughts on this? Do you believe the government should continue to declare the U.S. in a state of emergency due to COVID-19?
Personally, I commend the government for its handling of the pandemic. The implementation of vaccination campaigns, testing protocols, and treatment plans has been commendable. The availability of booster shots is a testament to the ongoing efforts to curb the spread of the virus and protect public health. I believe these measures have played a crucial role in mitigating the impact of the virus.
While I acknowledge that COVID-19 mutations and variants are still a consideration, the fact that I feel well after receiving the booster is reassuring. I think it’s essential to strike a balance between vigilance and a sense of normalcy. What’s your perspective on the current state of the pandemic and the government’s response?


katealyst
Hi Alexoskeleton! Thank you for pointing out that there have been 50 mutations of the Omicron variant. That is so surprising. I like the use of statistics throughout your post. In answering your question asking if I believe the government should continue to declare a state of emergency, I would agree with you and say no. The article linked below shows all of the declarations related to COVID during the state of emergency in 2020. Specifically, the state of emergency covered payments for COVID testing. While this was extremely important during 2020, I think it is less important now because the cases of COVID are not as deadly. People should continue to get vaccinated whenever a booster shot comes out and this should be paid for similarly to how people pay for Flu Vaccines each year. Thank you for making me think about this question.
https://www.kff.org/coronavirus-covid-19/issue-brief/what-happens-when-covid-19-emergency-declarations-end-implications-for-coverage-costs-and-access/