COVID-19 has a plethora of underlying effects. However, researchers may have just identified the most dangerous long-term impact.
While researchers have been studying COVID-19 for the past two years, pharmacy technician Nola Sullivan of Kellogg, Idaho, has uncovered the virus’s extending underlying conditions. Sullivan faced an additional struggle as a result of being infected with COVID-19 last year, despite the virus’s long-term effects, which included a loss of taste and smell, nausea, and diarrhea. Many COVID-19 patients too are grappling with an additional struggle: the onset of diabetes. In a research involving nearly 3,800 patients infected with the virus, cardiologist James Lo and colleagues discovered that just under half of the patients acquired elevated blood sugar levels that were not previously present. How is it conceivable for COVID-19 patients to develop diabetes? Many researchers have been tackling this exact issue for a long time.
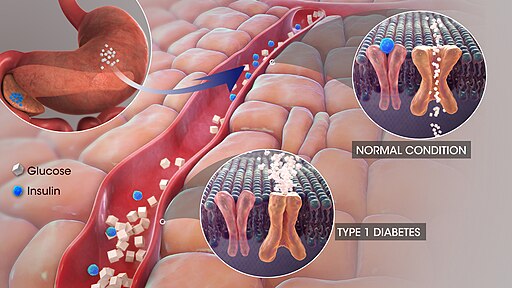
When a patient develops diabetes, he or she must learn to control the illness and live an active life due to an insulin shortage. Because diabetes is incurable, the prospect that it is a long-term side effect of COVID-19 is very troubling. Insulin is essential in the human body because it lowers triglycerides by boosting lipoprotein lipase activity, which degrades triglycerides into glycerol and fatty acids. A lack of pancreatic B-cells, which release proper quantities of insulin, has a direct impact on mitochondria and the glycolysis process which is utilized for energy synthesis by all cells in the human body, eventually prompting the pyruvate product to join the Krebs cycle for ongoing energy production. Both processes are required for continual energy generation. Glucose is broken down into pyruvate and energy during glycolysis. The process can take place in the absence of oxygen, making it anaerobic. Insulin promotes glycolysis by raising the rate of glucose transport across the cell membrane and the rate of glycolysis by boosting the activities of hexokinase and 6-phosphofructokinase.
Nonetheless, people with COVID-19 have experienced sugar surges. The elevated blood sugar levels were new after infection for the majority of the patients, suggesting that many of them had not been diagnosed with diabetes prior to contracting the virus. According to Lo and other experts, the mechanism by which COVID-19 causes diabetes is currently being investigated. Patients with ARDS caused by COVID-19 and a high blood sugar level were in the hospital three times longer than those with normal blood sugar levels. While the exact cause of diabetes is unknown, researchers have discovered evidence that the coronavirus attacks pancreatic B-cells, which produce insulin. This does not yet address the question because patients who received COVID-19 continued to generate significant amounts of C-peptide, indicating that pancreatic cells were still generating insulin. Despite this, their blood sugar levels remained elevated, suggesting that something else was at fault. The virus-infected fat cells must be stimulating other cells in a detrimental way, resulting in diabetes. As a result, Lo and colleagues observed that individuals with COVID-19 had low amounts of adiponectin, a hormone generated by fat cells that helps other cells respond to insulin’s urge to take up sugar. COVID-19 can clearly infect fat cells. The virus may also cause replication in human fat, which provides another indication as to how fat is implicated in the virus and, as a result, diabetes. While obesity has a significant impact on the onset of diabetes as a result of the virus, this is not always the case. The miscommunication of fat cells is to blame.
How may fat cell miscommunication be controlled, and who is directly affected? This is the next question that has to be addressed in order to develop a deep understanding of the long term effects of the virus.




cytokinesav
In a time where there is so much uncertainty regarding COVID’s aftereffects, I really appreciate your research topic. I feel it is directly related to our class and our knowledge of B and T cells in relation to diabetes. I didn’t know, however, the exact relation to the glycolysis process! Now I know the role that insulin plays in it and how diabetes takes part in interrupting the process. The virus can directly attack insulin-producing structures in the pancreas.
My father is a COVID specialist and told me about this phenomenon. Scientists still don’t have a direct answer as to why. It’s cool to learn about the sugar surges in COVID patients. Having done further research, I found that “hyperglycemia-having high blood sugar levels-is common in hospitalized COVID-19 patients and is strongly associated with worse outcomes…by disrupting fat cells’ production of [hormone] adiponectin” https://www.news-medical.net/news/20211002/COVID-19-may-trigger-hyperglycemia-by-disrupting-key-metabolic-signals-to-cause-severe-disease.aspx#:~:text=In%20the%20study%2C%20reported,associated%20with%20worse%20outcomes. Another further theme in COVID patients would be severe lung dysfunction as well.
I’m going to go home to tell my dad about this at dinner! Thank you for the insightful information in relation to our class.