Do you know someone who has sickle cell or has passed away at the hands on sickle cell? Well, new treatments using CRISPR technology are under way. This revolutionary treatment is made to last much longer than previous gene editing treatment, which lasted for up to a year. This treatment is called exa-gel made by Vertex and CRISPR.
How Does It Work?
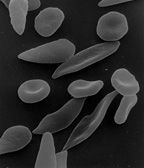
In sickle cell anemia, mutations in a gene HBB causes a change in the hemoglobin’s structure, causing circular red blood cells to twist into a sickled shape. The sickled red blood cells cause extreme pain and fatigue. In severe cases, beta-thalassemia can occur. Beta-thalassemia causes not enough hemoglobin or red blood cells to be produced, leading to low oxygen levels. The exa-gel technology targets the hemoglobin protein. It directs the Cas9 enzyme to the BCL11A gene and cuts its DNA off, turning it off. It is then able to produce fetal hemoglobin with normal shape. For this to be done, physicians must remove the bone marrow stem cells, edit them with the exa-cel, destroy the untreated bone marrow, and reinfuse treated cells. In AP Biology, we learned how the regulation of gene expression works. A gene that is usually on but can be turned off is a repressible operon. The operon regulates genes with the help of enzymes. The operator site is where repressor proteins can bind to turn off production. It is in between the promoter and structural genes. Usually, RNA polymerase binds to the promoter to begin production. Once that occurs, mRNA is transcribed. Then, tRNA picks up amino acids and the anticodons bind to the codons for the polypeptide chain to form. Finally, proteins will be produced to allow for the desired outcome to occur. However, Cas9 inhibits this process so that these sick blood cells will not be produced and healthy fetal ones will begin production.
The Future
While this new technology seems exciting, there are a lot of uncertainties about it. First of all, “the participants have only been tracked for a short time and that problems could arise later.” Although we do not know much about the long term effects of the treatment, we do see promising results. 29/30 of participants with sickle cell anemia reported no pain for a year after the treatment. 39/42 of beta-thalassemia no longer needed blood or bone marrow transfusions for a year after it. Sadly, it is expected for the treatment to cost about $2 million per patient. Due to this absurdly high cost, scientists are looking into a technique called haploidentical transplant to treat sickle cell anemia. This technique, which is also used for cancer, involves replacing a patient’s bone marrow with a parent or sibling who shares 50% of their DNA. 88% of patients with this procedure made normal red blood cells 2 years after it. This procedure is promising and much more cost effective; it could be popular in low income countries. Nevertheless, this new technology is extremely exciting and potentially world altering.



Leave a Reply