In March 2020, our planet was invaded, as we were threatened by the very initial strain of the SARS-CoV-2 virus. This event was commonly referred to as the Coronavirus pandemic. Little did we know then that there would also be several increasingly virulent variants facing us in the immediate future. This highly infectious and adaptive virus forced virtually everyone on Earth to quarantine and patiently wait for a worldwide team of multi-disciplined scientists and medical practitioners to develop an approvable and effective vaccine. For at least a year, we sat before our TV sets and awaited the daily numbers of the newly infected, hospitalized, and deaths. Populations throughout the world were being sent to hospitals in an effort to survive this dangerous virus. The hospitals and healthcare workers across the globe were stretched way beyond capacity, and the untold emotional effects on care providers, in itself, reached epidemic proportions.

The SARS-CoV-2 virus enters and attacks our lungs through our normal respiratory process. The virus causes our lungs to become inflamed, making it challenging for us to breathe. This can lead to pneumonia, an infection of the tiny air sacs inside your lungs where your blood exchanges oxygen and carbon dioxide. These viral effects made it difficult for middle-aged and older adults to cope and often left them vulnerable to the disease. Once the vaccines were advancing to a stage of government approval and being administered to the general population, we began to see statistically significant improvements in the overall ability of our immune systems to “take on” the virus and win the battle. As people were receiving the vaccine, most people were choosing the mRNA vaccines. These vaccines teach your cells to produce a harmless piece of the coronavirus spike protein that triggers an immune response to build antibodies. A spike protein is a specialized combination of amino acids designed to help the immune system know how to respond to the spike protein. In this way, one begins to build immunity to COVID-19, which results in mitigating the adverse effects of the virus or, in some cases, not succumbing to the effects of the virus. Once it does its job, the mRNA quickly breaks down, and the body clears it away in a few days.
All vaccines leave the body with a supply of T-lymphocytes and B-lymphocytes that will remember how to fight that virus in the future. Since COVID-19 is highly adaptive, as evidenced by the emergence of its numerous variants, biomedical researchers have to quickly produce a new vaccine to prevent a new SARS-CoV-2 virus variant from spreading.
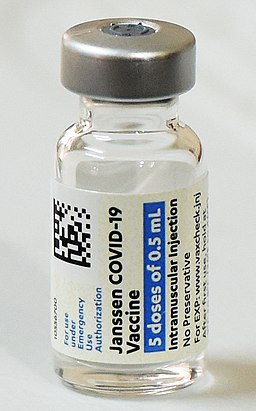
New concerns are now arising in the medical community with the threat of yet another new variant strand of SARS-CoV-2 emerging onto the scene as winter approaches. According to the Centers for Disease Control and Prevention, we could be looking at two new omicron subvariants becoming increasingly more dominant in the United States, raising fears that they could start another surge of COVID-19 infections. The new subvariants known as BQ.1 and BQ.1.1 are raising concerns because it appears to be proficient at evading the defenses of currently available vaccination formulations. According to the CDC, in recent weeks, BQ.1 and BQ.1.1 has quickly risen to 44% of all new infections nationwide and is approaching nearly 60% in some parts of the country, such as New York and New Jersey. Additionally, this viral landscape takes on even greater significance as we seem to be in a “viral trifecta” with the more common Influenza (flu) Virus and the Respiratory Syncytial Virus (RSV) taking the stage front and center this Fall and Winter season. Perhaps the best advice is to see your health care practitioner and see if a vaccination or booster shot is right for you!


Leave a Reply