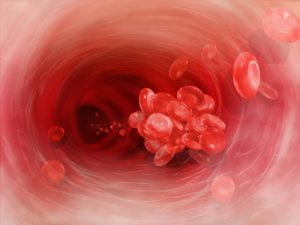
According to an article by Erin Garcia de Jesus, a new study shows that some of COVID-19’s lethal blood clots may originate from the immune system attacking the patient’s body instead of the virus. These clots form due to excessive inflammation from an overactive immune response in severely ill patients. Researchers are now trying to figure out how this response happens. Currently, the belief is that some of the clottings may come from auto-antibodies that go after the cell membrane-forming molecules instead of the foreign invader. This attack would prompt neutrophils to release a “web of genetic material geared at trapping virus particles outside the cells.” While this process may control infections in tissue, it causes clotting in the bloodstream. Cardiologist Yogen Kanthi and her colleagues at the National Institutes of Health in Bethesda, Md., reported that “some blood clots may form when the webs trap red blood cells and platelets, creating a sticky clump that can clog blood vessels.” Blood clots in the lungs have become a significant cause of death for COVID-19 patients.
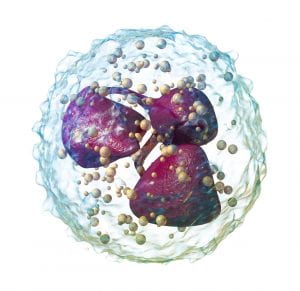
Auto-antibodies that recognize phospholipids can cause antiphospholipid syndrome (APS). APS is an autoimmune disease in which auto-antibodies can activate clot-forming cells, putting patients at a higher risk of blood clots. Extremely ill COVID-19 patients sometimes have high levels of neutrophils as well as phospholipid-binding antibodies in their blood. The belief is that antibodies may be causing the neutrophils to release traps that create clotting.
According to the study, of 172 hospitalized COVID-19 patients, more than half had auto-antibodies that recognized one of three various types of host phospholipids. When the researchers combined auto-antibodies taken from six COVID-19 patients with lab-grown neutrophils, the neutrophils cast their nets. Furthermore, when the researchers injected the same patient auto-antibodies into mice, the mice formed blood clots.
While this research is promising, Thomas Kickler, a hematologist at Johns Hopkins School of Medicine, states that “it’s unlikely that phospholipid auto-antibodies are the whole story.” Other inflammatory immune responses can also trigger clots, so the antibodies may only be part of the mystery.
On a brighter note, a process called plasmapheresis (filtering the liquid part of blood), could assist severely ill COVID-19 patients by removing the problematic antibodies.
This topic relates to our AP Biology study of the immune system. COVID-19 is a threatening virus that penetrates our immune system, and it can cause various problems in our body once it makes its way past our defenses. One of our main defenses is antibodies. Antibodies are specialized, Y-shaped proteins that bind to a foreign invader inside the body. The immune system uses the antibodies to search and mark the invader. Antibodies are a humoral response in part of the adaptive immune system which learns to recognize and eliminate specific invaders. People recovering from COVID-19 may have antibodies that are effective against the virus. Another bodily defense system is inflammation. Inflammation is an internal defense that is part of innate immunity. During inflammation, cells release histamine, and macrophages secrete cytokines. The histamines dilate local blood vessels and increase capillary permeability and cause the area to swell with fluid. Cytokines attract neutrophils and dendritic cells, and natural killer cells kill damaged or infected cells. A fever (a common symptom of COVID-19), is a systematic inflammatory response triggered by pyrogens released by macrophages.


Leave a Reply