Greetings, health explorers! Today, we’re diving into the twists and turns of a new study that unveils what happens in the aftermath of COVID-19. To put this into context, let’s picture this: you have now gotten rid of COVID from your body after suffering for a few days, but the health challenges still linger. A fresh study with 140,000 US veterans reveals how risks, from diabetes to fatigue, can play the long game for at least 2 YEARS! Crazy right?
The research revealed that patients initially hospitalized during their COVID-19 cases were more likely to experience these health problems. However, even those with milder initial infections were still at a higher risk for about one-third of the analyzed medical issues compared to those who didn’t test positive. The most common problems align with long COVID symptoms such as fatigue, memory problems, loss of smell, blood clots, metabolic issues, and gastrointestinal problems. The study found that for every 1,000 people infected with the coronavirus, a cumulative 150 years of healthy life is lost due to persistent symptoms, highlighting the significant impact of long COVID.
The article notes limitations. Some of these limitations include relying on electronic health records and potential skewing due to the predominantly male and older veteran population analyzed. It also did not include individuals who may have been infected but did not receive a positive test result in the early stages of the pandemic when testing was limited.
Wow, the impact of COVID-19 on long-term health is truly eye-opening! What are your thoughts on how we, as a society, can better address and manage the challenges posed by Long COVID? Share your insights below!
To set the stage, the World Health Organization (WHO) defines Long COVID, also known as Post-COVID Conditions, as the persistence or development of new symptoms three months post-initial SARS-CoV-2 infection, lasting at least two months with no other explanation. The Centers for Disease Control and Prevention (CDC) expand on this, noting that Long COVID encompasses a large variety of health issues affecting various body systems, even emerging after mild cases or in those who never tested positive for COVID.
Delving into the ideas, Dr. Akiko Iwasaki of the Yale School of Medicine and director of the Yale Center of Infection & Immunity, underscores that Long COVID is NOT A singular disease. Her research puts forward 4 hypotheses, suggesting that persistent virus remnants, autoimmunity triggered by B and T cells, reactivation of dormant viruses, and chronic changes post-inflammatory response may all contribute. 
In AP Biology, we learned about the immune system and B and T cells. The immune system plays a crucial role in identifying and eliminating pathogens, but in some cases, remnants of the virus may persist. This situation involves the adaptive immune response, where B and T cells are responsible for recognizing and responding to specific pathogens. Autoimmunity is triggered by B and T cells. The immune system is designed to recognize and target foreign invaders. Sometimes, it can mistakenly attack the body’s own health cells, leading to autoimmune disorders. B and T cells are crucial to the adaptive immune response.
How have your studies or interests in biology influenced your understanding of topics like the immune system and the function of B and T cells? Share your insights! 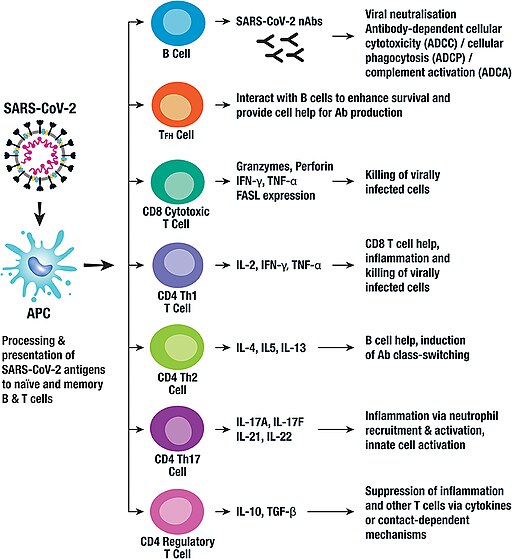
Some statistics addressed in the Yale Medicine article, address the question of Long COVID’s trajectory, the Household Pulse Survey in the U.S. shows a potential decline, with reported symptoms dropping from 19% in June 2022 to 11% in January 2023. The true prevalence remains elusive, with estimates suggesting 65 million affected globally, potentially underreported due to the rise in at-home testing since 2022.
Now, let’s connect this to the study involving 140,000 US veterans. The article showcases the persistent health risks associated with COVID-19, unveiling that even individuals with milder initial infections face a higher risk of enduring medical issues. Some problems at the top of this list include: fatigue, memory problems, loss of smell, blood clots, metabolic issues, and gastrointestinal problems.
For every 1,000 people infected, the cumulative loss of healthy life due to persistent symptoms amounts to a staggering 150 years. While the study acknowledges limitations, like reliance on electronic health records and potential population skew, it underscores the importance of protecting ourselves from COVID-19, given its potential long-term health consequences, even from seemingly mild infections.
Long COVID demands continued attention, research, and comprehensive strategies for prevention and management. As we reflect on these findings, it is evident that understanding and addressing Long COVID is crucial.
What are your thoughts on this?
Shifting gears, another article from The Centers for Disease Control and Prevention (CDC) delves into new guidance for healthcare providers treating patients with post-COVID conditions. The term “long COVID” is introduced, emphasizing that these conditions can affect individuals regardless of their initial symptoms. The CDC highlights a broad spectrum of symptoms, including heart palpitations, cognitive impairment, insomnia, and post-exertional malaise (PEM). While primary care providers can manage many cases, the CDC warns against relying solely on diagnostic results. People with post-COVID conditions are advised to continue preventive measures, and COVID-19 vaccines are highly recommended. The guidance is subject to updates as more information becomes available.
The FAIR Health study mentioned in the CDC article, indicates that over 23% of COVID-19 patients experience post-COVID conditions, with pain, breathing difficulties, hyperlipidemia, malaise, and fatigue being common. Half of hospitalized patients developed post-COVID conditions, and there’s a higher risk of mortality following severe treatment, more so for hospitalized individuals. The American Academy of Physical Medicine and Rehabilitation admires the CDC’s guidance for improving healthcare responses for long COVID.
As I did my research surrounding a health challenge that stretches far beyond the initial impact of the pandemic, the significance hits close to home. It’s not just data; it’s the lived experiences of individuals moving through the long-lasting effects of COVID-19. This isn’t just a call to action; it’s a call for our collective attention, research efforts, and a compassionate response. This health issue isn’t confined to statistics; it touches the lives of millions worldwide, making it a cause that resonates deeply within us all.


Leave a Reply