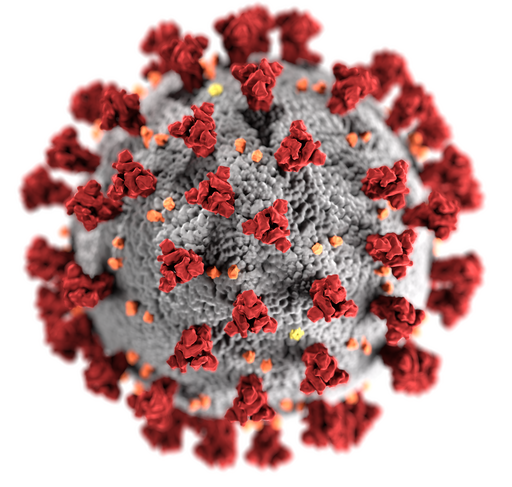
In the article I came across, it discusses how researchers have come across an ally within our immune system’s genetic coding. Human leukocyte antigen (HLA), otherwise known as the protein markers that signal the immune system, has been discovered to hold a secret that may revolutionize our approach to combating COVID-19. A specific mutation in the antigen, HLA-B*15:01, has emerged as a key player in asymptomatic infection of SARS-CoV-2. How did scientists stumble upon this discovery, and how does this mutation in the antigen actually allow infection without the presence of sickness?
Research conducted at the University of California, San Francisco (UCSF), led by Dr. Jill Hollenbach, didn’t hesitate to dive right into the genetic phenomenon, finding the very answers to those questions outlined above. Using a national marrow donor database and the COVID-19 Citizen Science Study (CSS) app, they tracked nearly 30,000 individuals through the first year of the pandemic, providing insights into genetic factors influencing COVID-19 infection and immune system-related reactions. In the end, the researchers revealed that a staggering 20% of asymptomatic individuals carried at least one copy of the mutated antigen HLA-B*15:01. Moreover, it was found that those with two copies were over eight times more likely to avoid falling ill.
The secret of these genetic guardians is actually quite simple, and, through collaboration with researchers from La Trobe University in Australia, the UCSF team focused on the memory T-cell – a key element of the immune system’s ability to remember previous infections. Through their exploration, the researchers found that individuals with HLA-B*15:01, even without previous exposure to SARS-CoV-2, demonstrated T-cell responses to a specific viral peptide (the NQK-Q8 peptide). The researchers then concluded that exposure to a kind of seasonal coronavirus, which carries a strikingly similar peptide to SARS-CoV-2 called NQK-A8, enabled T cells in these individuals to quickly recognize Coronavirus and mount a faster, and, overall, more effective immune response. This led to minimal – if any – presence of symptoms within the study.
Let’s link this research to what we’re currently delving into in our AP Biology class. In this unit in particular, we’ve been discussing and exploring the functions of cell signaling, as well as the ins and outs of the immune system. Thus, there are obvious associations between bodily response, antigens, and the immune system with SARS-CoV-2 to what we are currently uncovering in class. We learned how Helper-T cells kickstart the immune system by releasing cytokines that trigger mitosis in B – plasma B cells (which produce antigens) and memory B cells – and T cells – cytotoxic and memory. Knowing that this mutation in the antigen appears similar to SARS-CoV-2 NQK-A8 peptide, we can understand how this may have triggered an immune response in the past, and that a secondary infections would have been easier to take care of considering the memory B and T cells were already present in the body.
Can you see how it connects to what we’ve been learning in our AP Bio class? Isn’t our immune system fascinating? Let me know how you feel about this discovery!


Leave a Reply