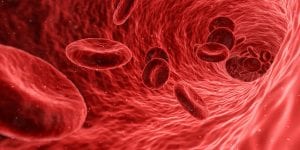
CRISPR gene-editing has recently been involved in the studies of sickle-cell anemia, a gene mutation that causes a decline in children’s health. Sickle cell anemia makes it difficult for oxygen to transport sufficiently throughout the body due to unhealthy blood cells. Some symptoms of the condition are shortness of breath, pale skin, colder body temperatures, headaches, etc…
Photo by SciTechTrend
Looking at sickle-cell anemia from a molecular standpoint, the mutation alters the red-blood cell by producing the wrong form of molecule which is referred to as a subunit. Out of the four subunits in hemoglobin, an “adult-expressed” subunit also known as “beta” is produced. In contrast, fetal subunits create “gamma” subunits which are the appropriate molecules in red blood cell development for children. The unfortunate results of a mutated gene are crescent-like and inflexible red blood cells, which can form blockages against the flow of blood and oxygen through blood vessels.
In the past, scientists have been able to increase the gamma production in hemoglobins by “reversing” beta subunits to gamma subunits through a form of therapy, yet in a recent study scientist dove deeper to prevent the mutation as a whole. With gene editing technology, CRISPR has been reported to be useful in putting an end to the hereditary mutation. In that, scientists can identify the mutation and cut the DNA target out by using CRISPR. A specific piece of the DNA, also known as the “control section”, is introduced to gamma subunits during a process of molecular conversion therapy and the ends of the control section are placed together after the mutated code for the gene is removed. Ultimately, this is said to reduce the adult-expressed subunits and stimulate higher levels of gamma subunits in fetal hemoglobins so that young children affected by sickle cell can avoid invasive treatments in their future.


Leave a Reply