The Infamous “14-day” COVID-19 Illness Has Still Not Ended for Some.
Approximately one in four COVID-19 patients appear to have lingering symptoms, even after they have fully recovered from the virus, says the University of California Davis Health. Known as “Long Haul Covid,” it has been relatively unknown why each person’s immune response differs drastically.
Feeling sick just two days after the world closed on March 11, 2020, my mom began to show all the symptoms of COVID-19. Tests were scarce, and by the time she was able to get one, it came back negative. However, she dealt with the severe and immediate symptoms of COVID-19 for six months straight. She maintained an on and off fever for months and has still not regained her taste or smell. Unsure of why everyone around her (including myself) contracted the virus and recovered after a mere 14 days, she searched for answers everywhere.
Luckily Dan Longo, Professor of Medicine at Harvard Medical School, published an article this past week in which he thinks he has discovered the reason. Antibodies mimicking the virus. You see, our body has a particular system for how it typically handles viruses.
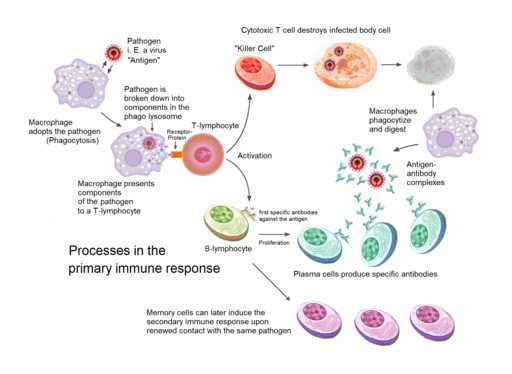
When pathogens pass the body’s barrier defenses, they trigger innate cellular defenses. In the area of entry, Mast cells release histamine and macrophages (large phagocytic cells), which secrete cytokines. These cytokines attract dendritic cells, which engulf the bacteria (COV2 virus) and fuse it with a lysosome to break it down, preserving the foreign antigen (epitope). The dendritic cell will then display the foreign antigen on an MHC protein on the cell’s surface. A T-helper cell will then come and identify the foreign antigen. Now activated, the T-helper cells will release interleukin (a cytokine) to signal the beginning of the cell-mediated and humoral response. In the Cell-Mediated immune response, the T-helper cells will stimulate other T-cells to divide and create two types of cells. T-memory cells will circulate your body to prevent reinfection, and Cytotoxic T-cells will kill any infected cells. In the Humoral Response, B cells will bind to the antigen on the virus and recognize it, while selected B cells will be stimulated by T-helper cells and divide. The divided B cells will become B plasma cells whose job is to secrete antibodies that bind to and neutralize the pathogen. Or B-memory cells whose job, much like the T-cells, is to circulate the body, preventing reinfection.
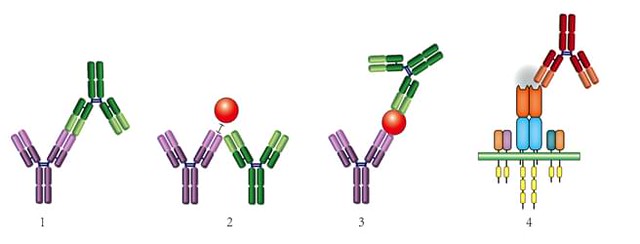
In regards to COVID-19, however, why hasn’t our immune response been consistent for everyone? Longo’s article answers that by closely drawing upon the concepts of Nobel Laureate Niels Jerne’s Network Hypothesis, in which she states that, as usual, the B-plasma cells produce protective antibodies in response to an antigen. However, these same antibodies later trigger a new antibody response, only this time toward themselves. These secondary antibodies are called anti-idiotype antibodies, and they are created when one antibody binds to the set of unique epitopes of another antibody. These secondary antibodies bind to and deplete the initial protective antibody response, mirroring the original antigen itself. Quoted from Longo’s research partner UC Davis Vice-Chair of Research and Distinguished Professor of Dermatology and Internal Medicine William Murphy, “A fascinating aspect of the newly formed anti-idiotype antibodies is that some of their structures can be a mirror image of the original antigen and act like it is binding to the same receptors that the viral antigen binds. This binding can potentially lead to unwanted actions and pathology, particularly in the long term.” Binding to the ACE2 receptor, an angiotensin-converting enzyme identified as the receptor for the SARS-CoV-2 viral entry, the anti-idiotype antibodies could affect normal ACE2 functions. With a lack of research surrounding the theory, Murphy states that he believes some of the long-lasting effects of COVID-19 reported result from the critical tasks of ACE2 being tampered with. In terms of the vaccine, most of the research studies on antibody responses focus on initial protection instead of long-term effects. Thankfully, Longo concludes by saying that most of Murphy’s and his questions are testable and can be at least partially tested in their laboratory.
It has been 21 months since my mom first contracted COV2, and thankfully she is doing much better. However, causing much frustration, she has not fully recovered. Similar to an autoimmune disease, she has periods where she feels fantastic and periods when she struggles. And so, while the information about Long Haulers Covid has increased dramatically, it is evident that there is still much to learn.


Leave a Reply